European scientists used stem cells to grow embryo-like structures that will shed light on human development, researchers in Ohio developed a breathalyzer-type device that can test for COVID-19 infection in seconds, and an artificial eye developed by scientists in Hong Kong exceeds the abilities of previous bionic eyes — and maybe those of human eyes, too. All that and more in this week’s coolest scientific advances.
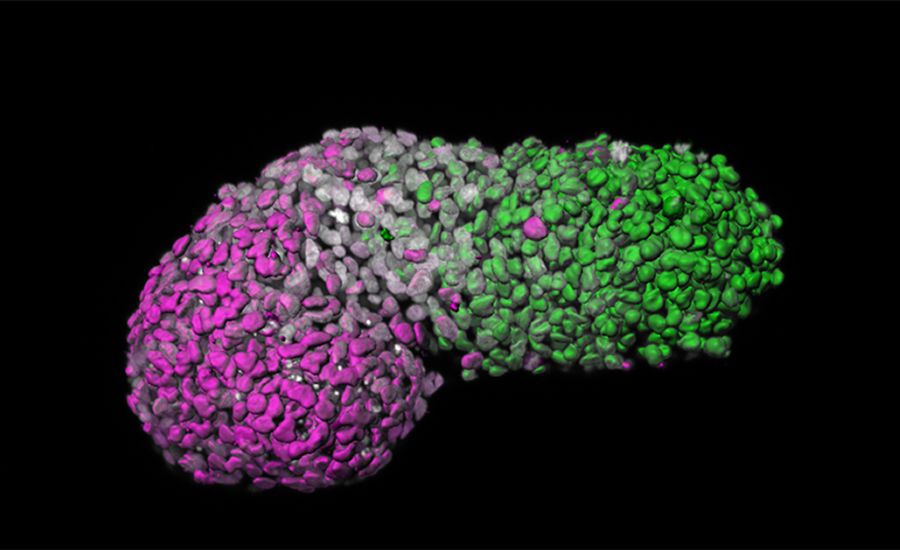
What is it? Scientists from the Netherlands’ Hubrecht Institute and the U.K.’s University of Cambridge have used stem cells to grow “embryo-like structures that mimic a crucial yet enigmatic stage of development.” Described in the journal Nature and in an accompanying article, these structures will allow researchers to model the development of a nascent human body at around 18-21 days after conception.
Why does it matter? Studying such structures could give researchers an unprecedented look at how the body develops at a key juncture — a process called gastrulation, when a homogenous ball of cells begins to differentiate itself into discrete body parts — as well as how certain developmental disorders arise, such as spina bifida and congenital heart conditions.
How does it work? As Cambridge notes in a release, gastrulation — which involves the development of three layers of cells that will grow into the nervous system, the muscles and the gut — is often called the “black box” of development: Legal regulations forbid the culture of human embryos beyond 14 days. In the lab, researchers were able instead to use stem cells create “gastruloids,” three-dimensional structures that differentiate themselves into the three layers that come to characterize the human body plan. Crucially, these gastruloids lack the components to form a brain or otherwise develop into a viable fetus, though — according to Nature — ethical questions may arise as scientists continue to develop more advanced structures.

What is it? The biotech company Moderna is set to begin the third phase of clinical trials of its vaccine against COVID-19. The randomized, placebo-controlled clinical trials will involve around 30,000 people.
Why does it matter? The primary goal of the trial is to demonstrate that the vaccine can prevent “symptomatic COVID-19 disease,” and a secondary goal is the prevention of severe symptoms requiring hospitalization in infected patients. Bloomberg reported on Thursday that Johnson & Johnson, which also has a vaccine in the works, expects to begin early trials in July — ahead of schedule — and that AstraZeneca and the University of Oxford are set to begin final-stage trials of their own vaccine this month.
How does it work? Moderna’s mRNA vaccine is, according to TechCrunch, “a technology that essentially provides instructions to healthy cells to produce antibodies to the coronavirus, without having to actually introduce any of the active or inactive virus itself.” The vaccine dose is set at 100 micrograms.
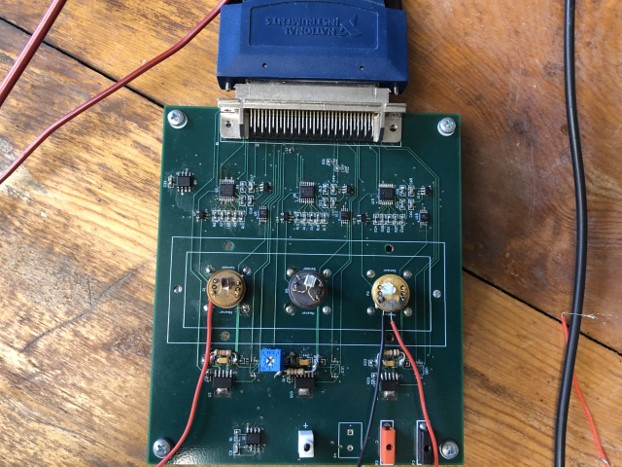
What is it? Researchers at Ohio State University are working on developing a breathalyzer-type device that could test for COVID-19.
Why does it matter? If effective, the device could offer a quick and inexpensive means of testing for COVID-19 that doesn’t require special training for personnel. Returning results within 15 seconds, it could be used to screen air travelers, for instance, or students as they enter the classroom. “The technology evolved from the sensors used for monitoring gases in an automotive exhaust, said Perena Gouma, a professor in OSU’s College of Engineering and director of the Advanced Ceramics Research Laboratory. “That’s how we started on breath analysis 20 years ago.” The COVID breathalyzer builds on a device Gouma invented to provide detection of the flu before symptoms appear.
How does it work? The handheld sensor reads nitric oxide in the breath as well as two other metabolites, according to OSU, that indicate the presence of COVID-19 even in patients who don’t show symptoms: “Exhaling once in the breathalyzer may help with earlier detection of the onset of the disease, as well as with monitoring of the severity of the infection, which could help reduce the risk for worsening of the symptoms and allow timely therapeutic intervention.”
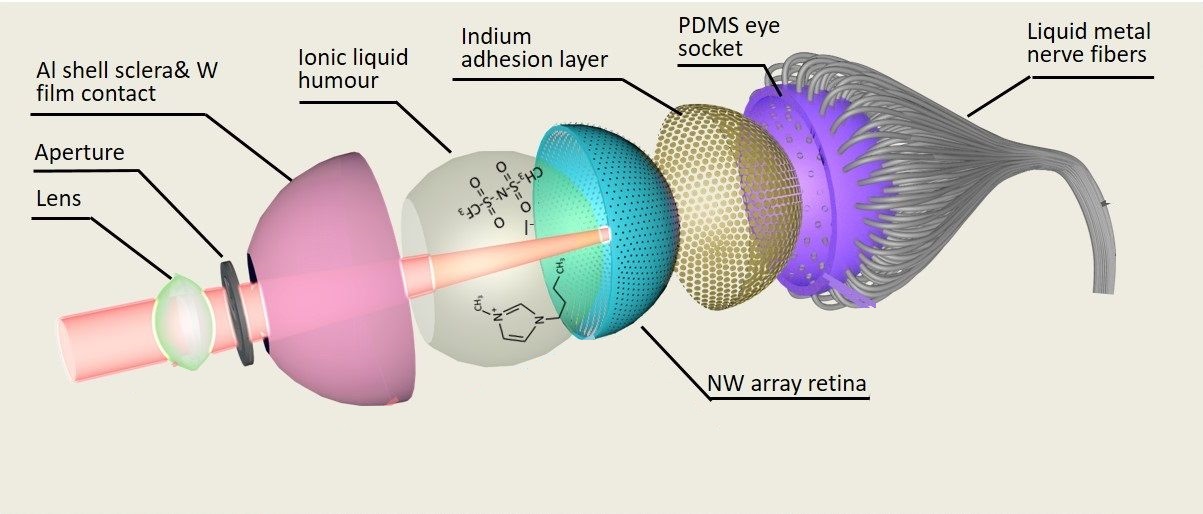
What is it? Together with colleagues from around the world, researchers at the Hong Kong University of Science and Technology (HKUST) have developed an artificial eye that can perform better than currently existing bionic eyes — and maybe better than human eyes, too.
Why does it matter? According to a release from HKUST, scientists have worked hard to replicate the “structure and clarity” of the human eye, but the current state of the art in prosthetic eyes still produces “poor resolution with 2D flat image sensors.” What HKUST researchers are calling the Electrochemical Eye, or EC-Eye, “not only replicates the structure of a natural eye for the first time, but may actually offer sharper vision than a human eye in the future, with extra functions such as the ability to detect infrared radiation in darkness.”
How does it work? The centerpiece of the new device is a 3D artificial retina, made from “an array of nanowire light sensors which mimic the photoreceptors in human retinas.” In the future, the researchers anticipate, the light sensors could be directly wired into the nervous systems of, for instance, patients with visual impairments.
What is it? Scientists from the Tokyo University of Agriculture and Technology found a way to synthesize cancer cells using diseased bladder cells from dogs, a development that will help researchers “diagnose cancer and optimize treatment without putting the patient through tiresome rigors of chemotherapy trial and error.”
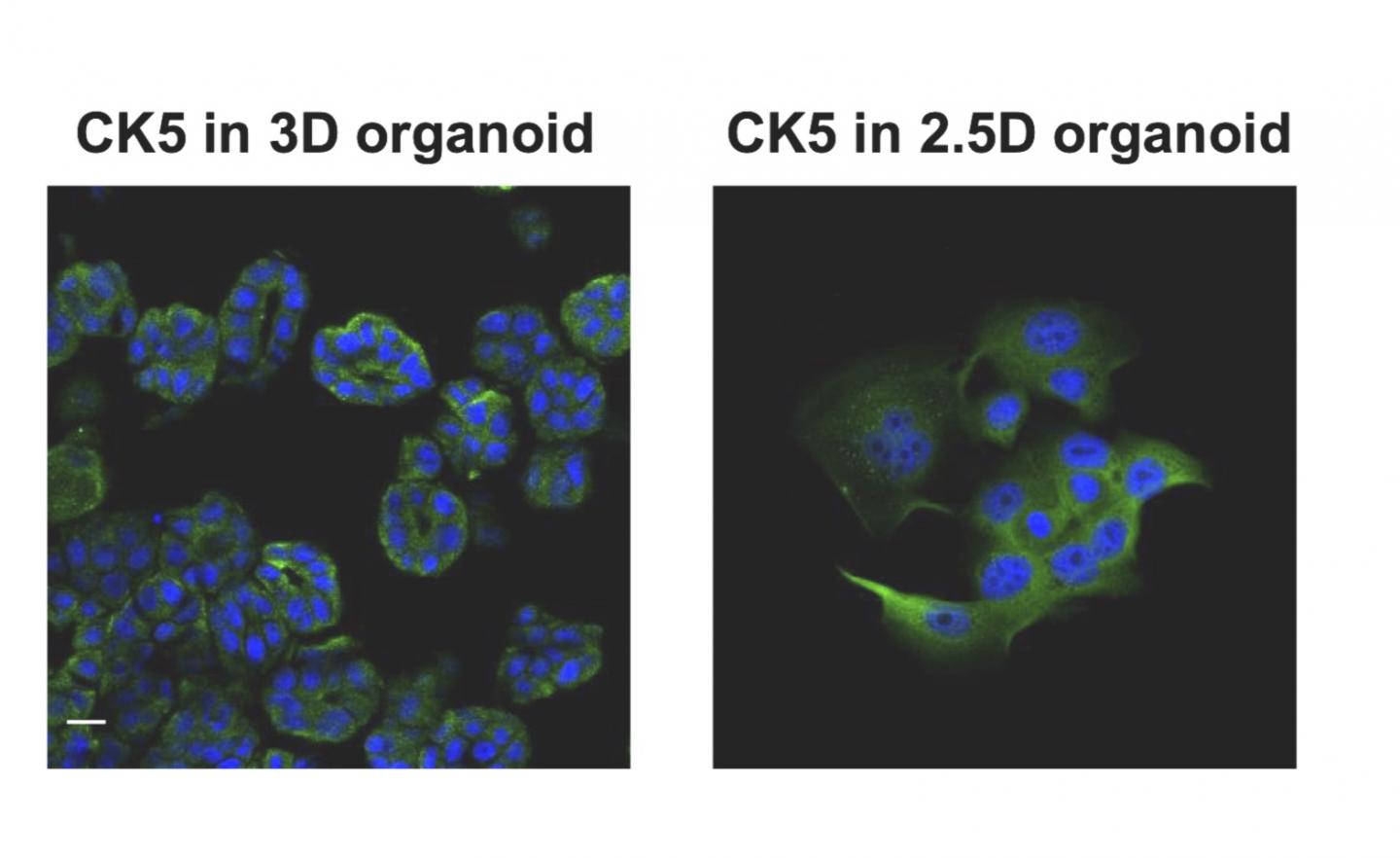
Why does it matter? The findings advance the field of organoids, which a recent article called “the new kid in cancer research” — it involves the creation of three-dimensional lab-grown cultures of cancer cells as a way of diagnosing cancer and developing therapies. But the process can be time-consuming, with costly materials. The Japanese researchers, describing their work in Scientific Reports, write, “Our newly established method overcame the issues of high cost and long handling time of organoids. Therefore, we believe that our established method becomes a promising research model for studying patient-derived cancer cells.”
How does it work? The researchers focused on bladder cancer in dogs because it occurs at a rate similar to human bladder cancer. As a release from the university explains, “They captured diseased cells voided in the dogs' urine and replicated them using a new process that generates bodies mimicking key characteristics of the original tumor cells closely enough that they can effectively be used to diagnose disease and identify possible treatments. The team created the organoids by culturing the captured diseased cells in a protein-rich medium.”